There are many reasons for our ignorance, both technical and ethical. Studying this period in human development requires obtaining ex utero samples at the termination of a pregnancy. However, women often do not realise they are pregnant during these first few weeks, and even if they do know and would be happy to donate their embryo for research, voluntary termination often only requires taking a pill. That means tissues extracted during surgery are rare, and tissues of sufficient quality to be used for research are rarer still.
The few samples that do exist provide the current gold standard for researchers working to understand human embryo development. But to really understand a system, thousands of examples are required and all the normal variance between individuals must be understood. Besides this, researchers would ideally be able to engineer the system, labelling or mutating its components to test different hypotheses. This is impossible with embryos derived from actual pregnancies (that is, from the fusion of an egg and sperm).
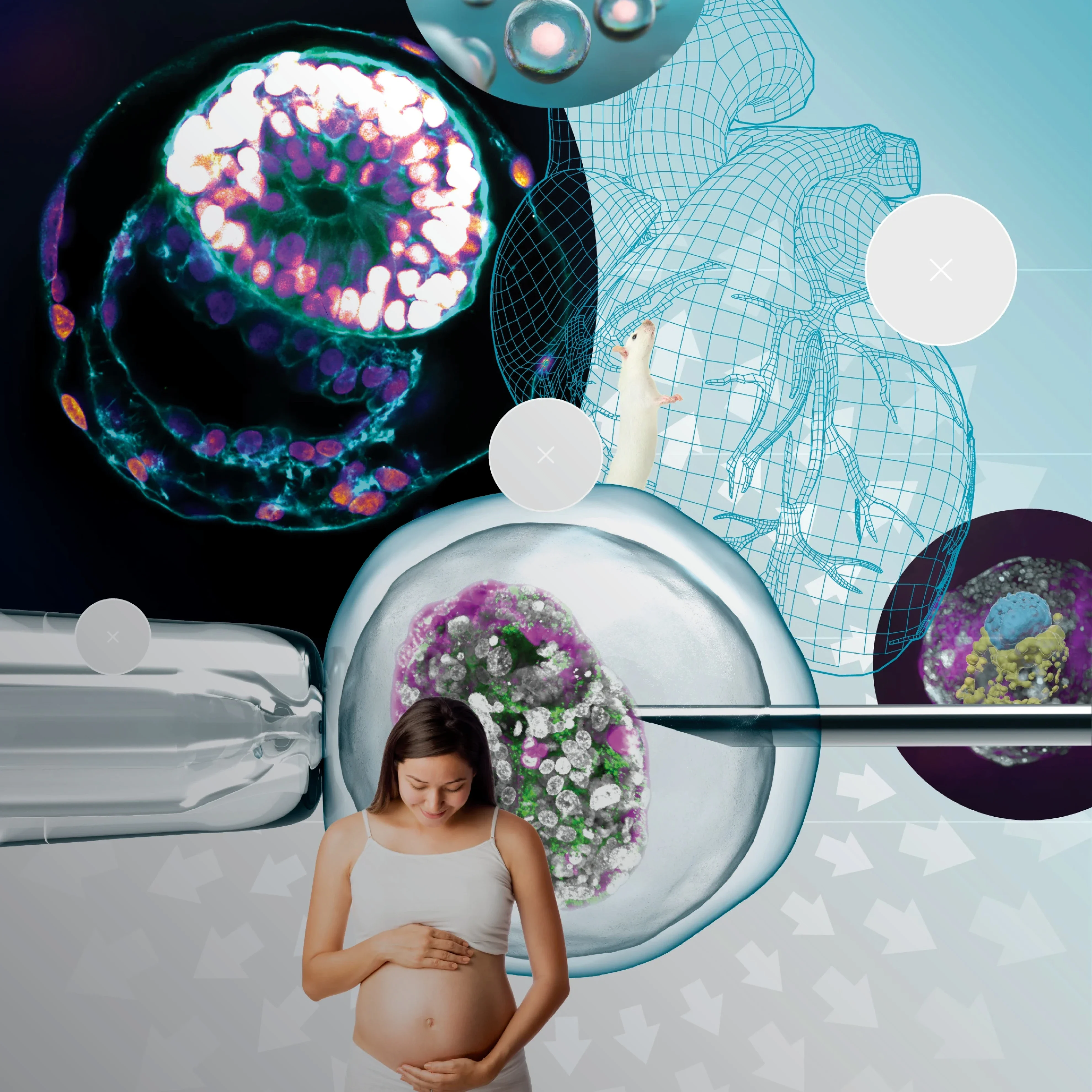
An alternative was required. Stem cells are a particular type of cell with the potential to divide to produce a range of different types of cells. Over the last few years, researchers have managed to steer stem cells to produce the functional units of an entire embryo, and subsequently to develop most of the structural organisation of a real embryo. By 2023 these embryo-like entities, or model embryos, had reached a point which allowed early human embryogenesis to be studied for the first time.1
Getting to this point required a huge multi-researcher effort over many years. The first challenge was that the stem cells needed to be highly plastic in order to give rise to both the embryonic tissues and the cells around the embryo, such as the yolk sac and placenta. Conventional stem cells are not capable of this, but around 10 years ago,2 we found a way to derive improved stem cells with extended potency which were able to do just that.
Second, we needed to be able to grow an embryo outside the uterus. We were able to develop this capability using animal models such as the mouse and rabbit. This was in itself a huge breakthrough for the field: such ex utero systems allow you to monitor the same embryo every day with your own eyes, which had never been possible before. This system gives researchers increased control, acces, and ability to observe and manipulate developing embryos.
But what happens if you take naïve stem cells and put them into the ex utero system? Using mouse cells and genetic engineering, we showed that you can grow embryo models that very closely resemble an 8.5 day-old embryo,3 meaning that they complete gastrulation — the process of making organ progenitors — and start making organs. Using human naïve stem cells turned out to be much easier, requiring no genetic-modification steps to encourage the formation of the different parts of the embryo. As well as being a pleasant surprise for the field, this was an interesting discovery in itself, demonstrating that human naïve stem cells are more plastic than those in mice.
However, only about 1 pe cent of human embryo models develop to the standard needed for useful research. Improving this efficiency remains one of the field’s biggest challenges, with optimisation of both the cells and the artificial uterus device required. How cells self-assemble into an embryo is primarily an architectural problem, and reliably replicating this in an artificial system will require advances in biomaterials science, bioengineering, metabolomics and microscopy. Physical constraints provided by the uterus are known to be important but are not well understood, and even the embryo’s own size is critical to development: many processes are directed through signalling molecules which diffuse through the embryo and organise it along different axes. If the embryo is too large, then the molecules may not reach far enough; if it is too short, they will be too concentrated to provide useful information to the cells.
There are also other fundamental biological questions, thanks to our ignorance of early embryonic development. For example, the placenta is essential to embryonic development in mice, but might not be in humans. As the models are used to try to answer some of these questions, the results in turn can be fed into improving the model system; the result is a positive feedback loop in which we both improve our understanding of human biology and refine our tools for investigating it.
In parallel to developing model embryo systems, scientists are also slowly building atlases of human embryonic development, collecting all possible data from the rare natural embryos obtained through pregnancy termination. These samples provide anatomical information about the developing embryo and can also provide information about which genes are turned on in its different cell types. Given how precious these samples are, it has become imperative for scientists around the world to deposit their data in shared, openly accessible repositories to maximise their value to research, both for the donor’s sake and for the public who fund this research.
Often when people hear about synthetic embryo models, they assume that researchers are trying to create embryos and replicate the whole course of pregnancy outside the womb. That is not the goal, nor is it actually achievable in any readily foreseeable timeframe. Embryo models are just that, models of structure and function, not viable entities that could become fetuses or babies. So looking ahead to the next 10 to 15 years, the dream would be to be able to take cells from a consenting adult and from these grow embryo models to day 40 with 80 per cent efficiency. Although only around 1 centimetre long, 40-day-old embryos are sufficiently developed for researchers to study the different embryonic structures and how organs originate. By using embryo models which can grow up to the same stage, we can knock out different genes to find out which are important for different processes, such as human liver development. We could also add alcohol, tar from smoke or administer different drugs to see how each affects the development of the embryo models. Using embryonic models from different species, we could compare human development to that of other animals and understand the similarities — and differences — in their mechanisms. This will give us the underlying principles of mammalian development in general, and also help us to understand data from preclinical trials in other species. Ultimately, synthetic embryo technology could be used in clinical trials to develop medical treatments and public health policies.
Beyond the practical limitations of trying to work with real human embryos, there are also a range of associated ethical concerns which can be addressed scientifically using embryo models. Restrictions on working with human and other primate tissues differ from country to country, making different strands of research more or less feasible depending on local guidelines. However, embryo models are still very different from real embryos, and these differences are not likely to disappear soon — they do not have the potential to grow to full-term pregnancy. This is due to both the technical restrictions of working in an artificial uterine system4 and how difficult it is to even encourage the cells to grow to a structured model of a few weeks old. Work is also under way to develop “restricted” stem-cell lines which cannot develop brain or heart tissues, decisively limiting their potential. Even if, in many years’ time, researchers did develop a way to support embryonic development to full term outside the uterus, the application of this technology would first go to supporting pre-term babies which would otherwise not survive, rather than replacing pregnancy to create embryos outside the womb.
Given the pioneering nature of this field, scientists are actively involved in developing ethical guidelines and policies to guide its future. One recent example is the UK’s publication of a voluntary code of practice,5 commendable for the breadth of expertise and perspectives involved. These guidelines provide good recommendations for the field, but given its fast-paced nature and different cultural considerations around the world, they will need to be interpreted flexibly and updated on a regular basis to take into account the latest research developments. However, development of international guidelines at such an early stage of research into synthetic human-embryo models will bring confidence to those working in the field, facilitate cross-border collaboration to accelerate research discovery, and provide both the transparency and time needed for the field to earn society’s trust and participation in decision-making.
This is important because there is an acute need for embryo models not just to satisfy our intellectual curiosity, but to improve human health. CMV infections — caused by the herpes virus — are very dangerous during pregnancy, but cannot be studied in mice, as CMV doesn't cross the mouse placenta. Certain brain-developmental disorders in children originate during embryogenesis; without embryo models, they are impossible to investigate and understand. And these are just the beginning; given our radical ignorance about early embryonic development, it is likely that embryo models will allow us to discover other, potentially enormously significant, processes and factors in the earliest and most sensitive stage of pregnancy.